NY and NJ: The Enduring COVID-19 Questions Around Nursing Homes
The days leading up to March in 2020 seemed like any other in New Jersey. COVID-19 seemed like an isolated virus or so that’s what Americans were led to believe. News coverage of the Coronavirus the month before had mainly focused on a Washington state nursing home where elderly patients were battling a fast-spreading respiratory illness.
By the middle of March, that nursing home, Kirkland’s Life Care Center, had lost several dozen of its frail patients to COVID. Americans watched gut-wrenching, video of family members touching the glass windows of the facility to comfort loved ones because they couldn’t go inside.
The haunting images have now come to symbolize the beginning of an unpredictable storm that engulfed the nation and pushed it into the kind of lockdown modern civilization had never seen before. New York became the epicenter of the Coronavirus in the United States. New Jersey gained the same unwanted designation, considering the regional connection between the two states. Beginnings are always difficult, especially when lives are at stake. Leadership means making sound decisions amid sheer chaos, hoping that in the end, the choices were the right ones.
New York Governor Andrew Cuomo and New Jersey Governor Phil Murphy, both Democrats, promised

to work together and keep the region on similar pandemic emergency plans. Cuomo’s administration was quick to issue a rule that stopped visitations at nursing homes. New Jersey did the same.
On March 25, 2020, Cuomo’s Health Commissioner Dr. Howard Zucker issued a controversial directive. The new rule, in part, read, “No resident shall be denied re-admission or admission to the NH (nursing home) solely based on a confirmed or suspected diagnosis of COVID-19. NHs are prohibited from requiring a hospitalized resident who is determined medically stable to be tested for COVID-19 prior to admission or readmission.”
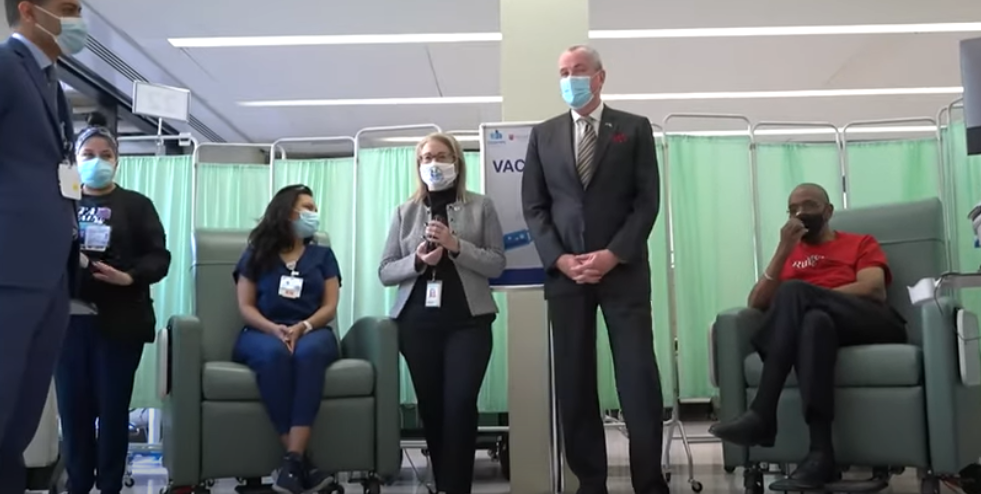
New Jersey adopted a similar directive on March 31, 2020, but with stipulations. Governor Murphy explained the policy at a recent COVID briefing. He says it was based on advice from his Health Commissioner Judy Persichilli.
“The directives were crystal clear about separating, different floors, different wings, different buildings, including for staff,” Governor Murphy said during the briefing. “Judy went one step further and said to all of the operators, ‘if you can’t do this, if you can’t abide by the directives, call me, call us, and we will help you find a safe solution.”
Close to 8,000 residents have died of COVID-19 at long-term care facilities and nursing homes in New Jersey, including Veterans Homes that are state-run.
A year ago, on April 1st, just a day after New Jersey’s directive, three organizations describing themselves as dedicated to preserving the safety of patients, residents and other staff at long-term care facilities, sent out a dire warning about New York’s directive.
In a joint statement, The Society for Post-Acute and Long-Term Care Medicine (AMDA), the National Center for Assisted Living (NACL) and American College of Health Care Administrators (CHCA) copied and pasted New York’s directive on to a press release and added a line that read: “We are deeply concerned with the recent New York State order.”
The organizations urged other states not to enforce this kind of policy. That wasn’t all. AMDA, NACL and CHCA offered COVID data from the Washington state nursing home that had faced unimaginable tragedy, and explained why a “blanket, one-size-fits-all approach statewide” could be dangerous.
“We strongly object to this policy directive and approach to developing surge capacity,” the joint statement read. “We are aware that other states may already be adopting a similar approach in order to free up hospital beds. This is a short-term and short-sighted solution that will only add to the surge in COVID-19 patients that require hospital care.
“Based on what we currently know about how this virus can spread in institutional settings, the hospitalizations and case fatality rate, this action by a state will put the many frail and older adults who reside in nursing homes at risk.”
The press release encouraged long-term care facilities to create separate settings for recovering COVID patients, including large field hospitals, dormitories, hotels and shuttered nursing homes or hospitals.
AMDA has chapters in both New York and New Jersey. The organization’s Executive Director Christopher Laxton tells InsiderNJ that despite the strong statement, neither New York nor New Jersey reached out to the organization’s chapters in both states.
“We offered help right at the beginning when we saw New York was a hotspot and this was regional,” Laxton said. “We reached out and personally wrote Governor Cuomo. Basically, zero response. It was like talking to a wall.
“There was a very bright line between health officials, who were advised by post-acute and long-term care clinical experts, and those state officials who were not.”
New York’s Dr. Zucker has defended his directive, saying it prevented the state’s health care system from collapsing. He has also maintained the policy wasn’t to blame for the spread of the virus but that staff members brought COVID into the facilities. New York, the subject of an investigation into COVID death numbers at nursing homes, lost 15,000 residents at its long-term care facilities.
Laxton agrees staff members were partly responsible for bringing the Coronavirus into long-term care facilities and nursing homes across the country. But he says New York and New Jersey’s refusal to have hospitals test patients during discharge didn’t help.
“A lot of caregiver staff go in and out of these rooms a lot,” he said. “We know the combination of staff, who live in the community, going home and coming back to the building, combined with the positivity rate in these communities, especially in ‘hot spots’ — that really is what contributed to the high rate of deaths.
“Back in March, we were just figuring it all out, a lot of nursing homes are small, how do you cohort in a situation like that? You have to set up an entire building. Most of them are older buildings with no upgraded ventilation systems.”
But Laxton says AMDA was able to make some headway in New Jersey in the summer. We reached out to Governor Murphy’s office for comment. Spokesperson Alexandra Altman referred us to Murphy’s public statements. During his March 22nd COVID briefing, Murphy said his administration has been re-examining actions taken during the pandemic at long-term care facilities and nursing homes.
“Judy had the courage, and I give her credit again, to hire an outside firm, completely independent, to hold a whole mirror on our process,” Murphy said, “Executive orders that were needed, laws that needed to be passed and signed, much of which has occurred.”
New Jersey’s Attorney General also launched an investigation into long-term care facilities, including Andover Subacute and Rehabilitation Centers, where 17 bodies were found crammed into a makeshift morgue. The office is also investigating state-run Veterans Nursing Homes.
“Does this mean that there were operators who may have ignored the directives and screwed up?” Murphy asked at his briefing, “It’s quite possible there were.”
The Governor also pointed out that returning patients had connections to long-term care facilities.
“This is where they live,” Murphy added.
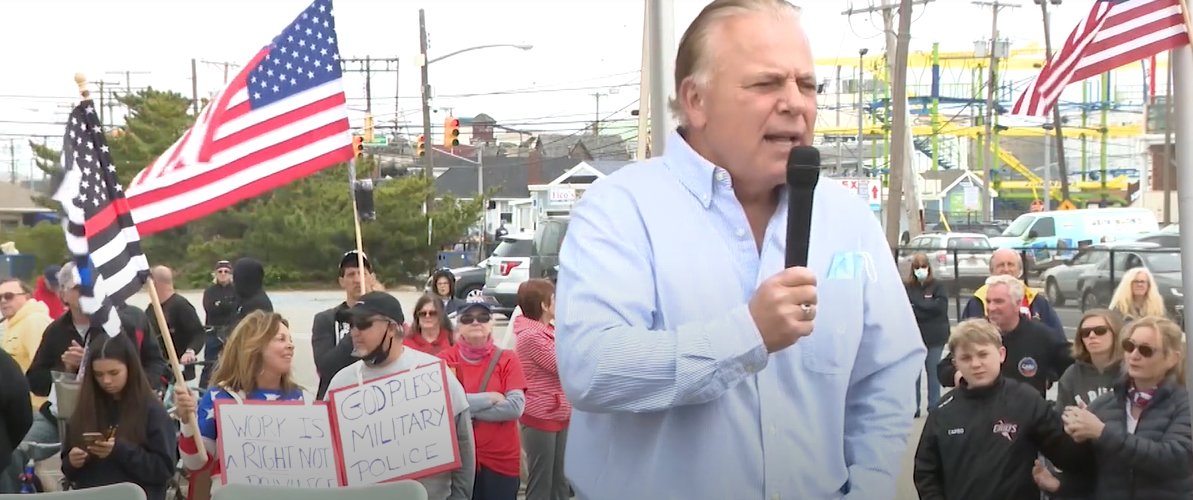
Republicans like New Jersey State Senator Joe Pennacchio, though, say it’s all a little too late. Pennacchio, who’s been sounding the alarm since the early days of the pandemic, says many deaths could have been prevented.
“They failed to protect the residents within these homes,” Pennacchio tells InsiderNJ. “They exacerbated the problem by admitting and readmitting patients into nursing homes not knowing they had COVID, and prohibited these patients from being tested.”
Pennacchio chaired a hearing on March 5th where lawmakers listened to testimony from family members who lost loved ones to COVID at nursing homes and long-term care facilities in the Garden State. Lawmakers also listened to a Veterans Home resident who watched his friends die of the Coronavirus.
Pennacchio, who is medically trained because he’s a dentist, says he wants to know why some state-run Veterans Nursing Homes barred employees from wearing protective face masks at the outset of the pandemic. He’s posed that question in a letter to Christina Tan, the state’s epidemiologist, and claims Murphy’s office helped enforce this rule.
“They were in charge of those three facilities and they failed,” Pennacchio said.
Murphy’s office again referred us to his public comments. The Governor has not directly addressed these allegations. Democratic State Senator Joe Vitale, who chairs the Health Committee, has been demanding answers.

“There were facilities and Veterans Homes that prohibited staff from wearing masks because it frightened their staff,” Vitale said. “I spoke to some staff at nursing homes and they were told not to wear masks. There was a shortage of PPE. It’s easy in hindsight to say we should have done A, B or C. We know a lot more now than we knew then.
“The state has acknowledged responsibility and it was through my efforts that some assistant CEOs were dismissed because everyone realized they didn’t protect the residents as they should have. It wasn’t woeful but careless and uniformed, but at the end of the day, someone has to bear responsibility.”
Laxton says former President Donald Trump also bears some responsibility. There was an inadequate supply of PPE and gowns during the height of the pandemic.
“All of this could have been solved with better Federal coordination and taking the virus seriously,” Laxton said. “States ended up competing against themselves to get access to masks, gloves and gowns.
“It was an abdication in leadership,” he added.
“Let’s step back and say we were clobbered, we lost thousands of people and we mourn the loss of every single one of those lives, and we weren’t alone,” Murphy said during his COVID briefing. “Every American state, as far I could tell, every country in the world lived with an awful reality in their long-term care facilities.
There is no question the most-populated states got “clobbered.” According to COVID tracking of nursing home deaths, California lost 12,869 to COVID at 2,000 long-term care facilities and nursing homes. California issued a similar directive to New York’s but rolled back on the policy.
Florida and Texas, both run by Republican Governors, weren’t spared, either. Neither state issued a directive. However, in Florida, 10,713 residents died of the Coronavirus at 1,900 long-term care facilities and nursing homes. In Texas, 10,373 residents died at 2,308 facilities.
“Other states benefited from our knowledge and how we responded,” Vitale said. “Florida, their numbers are less than ours because they were hit late and were better prepared. In other words, states that were late to get the virus should have been better prepared to respond.”
Health Commissioner Persichilli says the majority of residents at long-term care and assisted living facilities in the Garden State have received both doses of the COVID-19 vaccine. At long-term care facilities, more than 70 percent of residents are now fully vaccinated. At assisted living homes, that number stands at 90 percent. Persichilli, though, says the challenge now is that only 50 percent of staff at these facilities have accepted the COVID vaccine. The state’s launching a campaign to make sure everyone knows the vaccines are safe.
New Jersey and the Nation have learned deadly virus outbreaks are no longer something they watch unfold somewhere else. The question in the future won’t be whether the U.S. will face another pandemic, but rather, when it could happen again.
Laxton says all long-term care facilities and nursing homes need to make pandemic planning part of their emergency preparedness. That means building separate structures if need be, updating old ventilation systems and making sure there’s an ability to set up rapid isolation sections.
Laxton also says he hopes all state leaders reach out to his organization for advice.
“There are some states that have done better,” He said. “Maryland and Colorado had strong involvement from our members, and even the state of Washington, after the outbreak, started listening to our medical directors eventually.”
Laxton says staff members at all long-term care facilities and nursing homes need to be paid better, as well.
“These are largely folks who work two or three jobs,” Laxton said. “They could make more flipping burgers but they do this work because they love their patients, and their connections are with their patients and families.”
For his part, Senator Vitale has proposed legislation that would increase the pay of New Jersey’s Certified Nursing Assistants (CNAs). But both sides agree America as a whole needs to better protect its vulnerable, older citizens. In the face of adversity and terrible loss, it takes leadership to make that a top priority.
Letter to CuomoAMDA






Leave a Reply